While dental implants are highly successful and predictable when planned and executed properly, complications do occur. Over 90% of dental implant complications are often due to poor diagnosis, planning, and operator error in performing the procedures. Here is an example of a patient who requested removal of two implants because of continued pain and swelling as well as inability to get the second implant restored. He also lost sensation of his lower lip and chin on the right side. His X-rays clearly shows advanced bone loss and poorly positioned implants. 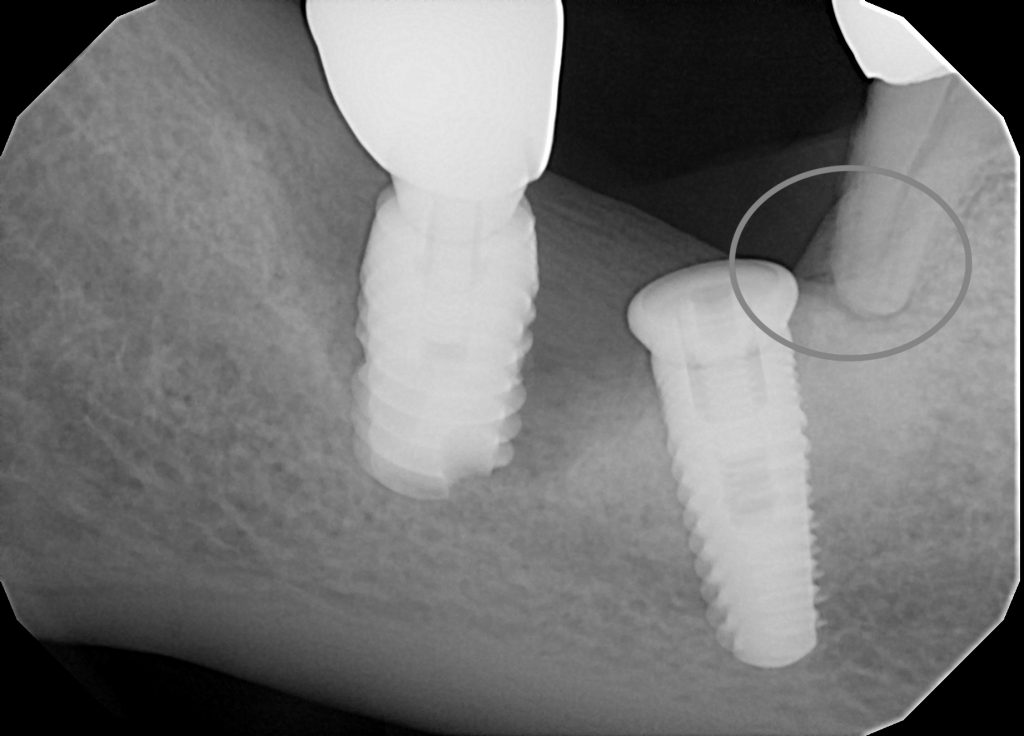
After reviewing the history of his treatments, the factors contributing to his implants failure became more apparent:
- No surgical guide used in placement of implants
- Implants were placed in already deficient bone that should have been augmented prior to implant placement
- No cone beam CT scan used for diagnosis
- No 3-dimensional planning performed
- No clear instructions on home care and professional hygiene after implant placement
- No attention to adjacent tooth with existing bone loss and periodontal disease (a big risk factor)
- Patient is a smoker! No patient education or discussion was ever given on effects of smoking on treatment outcome (another big risk factor)
The treatment sequence for a patient with such conditions includes a staged approach- first eliminating the infection and inflammation and its sources, then restoring the missing bone and gum tissue, and finally replacement with dental implants positioned properly for support of final restorations:
Stage 1:
- Atraumatic removal of dental implants using reverse torque technique
- Debridement and irrigation of all inflammatory and infectious tissues sites
- Extract adjacent tooth due to 100% loss of bone
- Place Platelet rich fibrin membrane in the site to promote soft tissue healing of the site
- Allow site to heal for 2-3 months
Stage 2:
- Cone beam CT scan to assess the bone anatomy: width and height
- Bone graft to restore width and height as much as possible to develop proper implants sites
- Enhance gum tissue as necessary to create good quality and quantity of soft tissue
Stage 3:
- Digital diagnostics and 3-D computer assisted planning for placement of the new dental implants
- Fabrication of implant surgical guide using CAD / CAM or 3-D printing
- Precise placement of dental implants according to the diagnostic work up.
- Allow 3 months of healing
Stage 4:
- Verify proper implant healing and integration
- Take digital impressions to begin design and fabrication of final restorations
- Fabricate customized abutments and restorations
Stage 5:
- Thorough patient home care instructions and education on effective hygiene practices
- Professional implant care and hygiene every 3-4 months
- Educate patient on risks associated with smoking and begin a cessation program.
There is no mystery to achieving success in dental implant therapy. It requires a team approach and thorough communication between the patient, surgeon, restorative dentist, lab technician, and the implant care practitioner / hygienist. It also requires methodical diagnosis, planning, and execution with attention to biology, anatomy, function, and aesthetics. And it all must meet patient’s expectations for their time and investment.
Dr. H. Ryan Kazemi is an oral and maxillofacial surgeon in Bethesda, MD
