There are several requirements for achieving success with dental implants and the aesthetic and functional results patients expect. These include presence of adequate bone and gum tissue along with precisely placed dental implants and biologically-compatible restorations that mimic natural teeth. With advances in tissue augmentation and digitally-driven treatment planning and implant placement, we can now predictably achieve such results and prevent many complications.
When basic principles of dental implant therapy are not followed, complications often do follow. One such complication is gum recession around dental implants leading to poor aesthetics, inflammation / infection (peri-implantitis), and ultimately implant loss. Gum recession is often caused by either lack of adequate bone or poorly positioned implants with excessive labial (i.e. front) angulation. Both lead to loss of gum tissue, exposure of implant surface, plaque attachment, formation of bio-film (bacteria and its toxins on implant surface), inflammation or infection known as peri-implantitis, further bone loss, and ultimately loss of the implant.
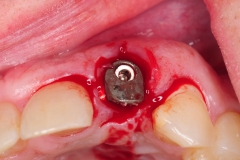
This patient presented with complaints of poor aesthetics and pain around his upper left dental implant. Examination revealed uneven gum tissue, pain on palpation, and purulence (pus) as well as deeply inflamed gum tissue. Cone beam CT scan showed a poorly aligned implant with severe inclination and lack of bone on its buccal aspect.
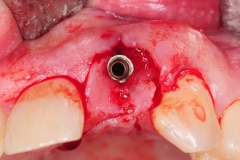
The only viable treatment in this circumstance is implant removal (explantation) and restoration of missing bone and gum tissue and replacement with a properly positioned dental implant and restoration. The implant was removed using reverse torque technique.
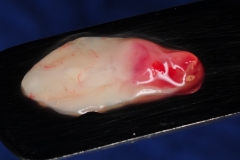
The site was cleaned, irrigated, and packed with platelet-rich fibrin (PRF) membrane obtained from patient’s own blood. The PRF membrane with its active growth factors promotes a more rapid healing of the site. A removable transitional prosthesis was then delivered. After 8 weeks of healing and natural regeneration of the gum tissue, the site can be assessed for bone development and eventual replacement with a new dental implant and restoration.
Management of such complications requires a staged process designed to eliminate disease, restore missing tissue, and replacement with a new dental implant in proper position. See example of a patient with revision therapy for gum recession around her lateral incisor.
Dr. H. Ryan Kazemi is a board-certified oral and maxillofacial surgeon in Bethesda, MD.