Dental implants have proved to be an effective and predictable tooth replacement option for millions of patients. The ability to eat and smile with restorations that resemble natural teeth has transformed the lives of many. However, a few patients report atypical symptoms described as ‘pressure,’ ‘an uncomfortable awareness,’ ‘feeling tired,’ or atypical signs such as headaches and skin rashes- even in absences of detectable disease or pathology around the implants. Having exhausted all medical and dental etiologies for their symptoms and with desperation to get relief, they choose to have their implants removed, believing their potential correlation.
Then comes the dilemma: Should patients with atypical health-related issues with no apparent reason, have their implants removed, and should dentists, without apparent disease or pathology, remove the implants?
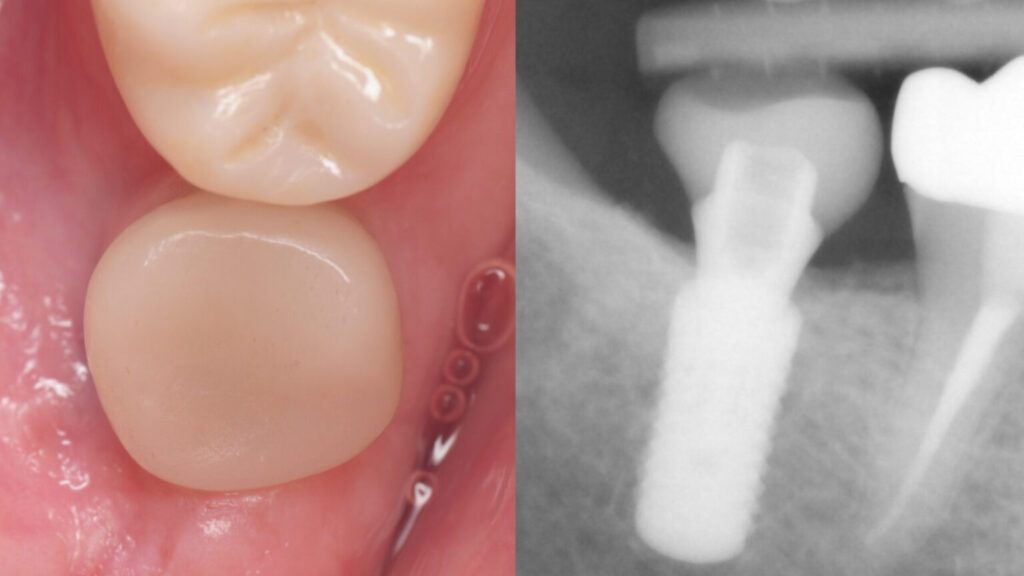
This patient complained of a ‘pressure’ sensation around the implant since its placement. The restoration was revised a couple of times with no change. Clinical and X-rays show a well-placed implant with completely healthy bone and gum tissue. Although the restoration appeared under-contoured, the implant had no specific problems. After two years, she finally asked her dentists to have the implant removed. Her dentists advised against it as they saw no issues with the implant. While such cases are sporadic, they present a debilitating situation for patients looking for a solution. The implant was ultimately removed in this patient and her symptoms resolved completely shortly after. The etiology remained unknown and we could not explain the precise reason for her improvement. We suspected poorly fitting abutment and restoration system or bite issues as possible causes. Revision therapy of the restoration was recommended but declined by patient who instead opted for its removal.
The dental literature lacked any specific protocol for managing dental implants with atypical symptoms. Hence, several years ago, we proposed the following treatment protocol, sequence, and philosophies for management of such conditions:
- A complete medical evaluation to rule out potential systemic diseases or abnormalities that might explain patients’ reported symptoms
- A comprehensive dental evaluation to assess the health of the teeth, existing restorations, existing implants, supporting bone & gum tissue, and bite. Evaluation requires both clinical and X-ray evaluation including cone beam CT scan. Restorative, endodontic, and surgical consultations are imperative.
- Any positive medical or dental findings should be addressed and treated.
- Removal of the implant restoration and replacement with a healing abutment or a prototype restoration and assess any possible relief of the reported symptoms
- Is there inflammation around the implant without bone loss or measurable gingival pockets? This condition is known as peri-implant mucositis, which is managed with proper implant debridement and cleaning to remove any biofilm.
- Is there inflammation around the implant with evidence of bone loss? This condition is known as peri-implantitis. Management strategies range from debridement, site bone graft, to implant removal if advanced.
- Is there questionable peri-implant disease not conclusive from clinical or X-ray evaluation? Consider a surgical exploration and visual assessment.
If a patient requests the removal of a dental implant without any other medical or dental etiology or implementation of any therapies without improvement, then:
- The treating dentists should discuss and present the findings and recommendations in verbal and written treatment plan.
- There should be clear communication regarding the possible outcomes of the implant removal, including no guarantee for improvement of the symptoms in the absence of pathology or disease around the implants.
- The treating dentists must review informed consents indicating the condition, diagnosis, treatment options, and possible outcomes of the implant removal.
- Perform an atraumatic reverse-torque implant removal technique to minimize damage to surrounding bone and soft tissue.
- Regenerate bone at the site of implant removal by socket preservation /augmentation techniques.
- Routine follow-up to assess healing of the site as well as changes in symptoms.
How about the ethics of removing a healthy dental implant? For years, many clinicians felt it was wrong to perform such a procedure in the absence of disease just because patients requested it. While this is an ongoing conversation with perspectives on both sides, let’s consider the following: Patients consent to have implants placed. They certainly have the right to have them removed, providing clear communication on expectations and treatment outcomes.