A question often asked by some clinicians when planning for dental implants, is whether to use a prefabricated abutment or custom abutments. Some clinicians use prefabricated abutments to lower cost and eliminate the time required for a custom impression. The fact is prefabricated abutments are very limited in their use and are inappropriate for most sites. This is because they do not provide the proper support, emergence profile, and contour for the restoration. As the result, patients often complain of unaesthetic crowns and problems with frequent food impaction.
To achieve highly aesthetic, functional, and hygienic dental implant restorations, the following are required:
- Adequate bone width and height
- Adequate soft tissue thickness
- Proper implant width
- Precision implant position, angle, and depth
- An abutment that follows natural tooth anatomy at the gingival interface, i.e. custom abutment
- A crown that has proper contour and marginal integrity following the emergence of the abutment
- Proper anatomy of the abutment and crown at the embrasure space to support the papilla
Dr. Benjamin Watkins, a renowned Washington DC prosthodontis, says: “In the esthetic zone, the use of custom abutments is an absolute must. There is no better way to create acceptable subgingival contour that matches that of a natural tooth. In addition you cannot adequately control the position of the margin with a stock abutment, which can place you at higher risk of subgingivally trapping definitive cement. This a silent but potentially catastrophic issue because once it is there it is often very difficult to remove it. Many times a clinician may not be aware that this has occurred until many months after the restoration has been placed.”
He adds: “The long-term implications of subgingival margin placement and inadequate cement removal can lead to complications such as soft tissue inflammation, gingival recession, esthetic failure, loss of peri-implant hard tissue and bone loss on an adjacent natural tooth. The risk factors of using a stock abutment far outweigh the financial saving gained by using them, regardless of the location in the oral cavity.”
Dr. Watkins further says : “CAD/CAM custom abutments allow the clinician to approve the position of the finished margin prior to the milling of the final abutment. Therefore, it is advisable to have the clinician’s laboratory technician allow access to the final virtual design prior to milling the final custom abutment. This is a tremendous advantage to the clinician because it allows full control of the subgingival contours, position of the definitive margin as well as height, width and angle of the final preparation.“
In selecting a custom abutment, the restorative dentist must pay close attention to clinical requirements and appropriate contours of the restoration to achieve the desired result. They should precisely assess the size of the space, occlusal table, relationship to opposing arch, soft tissue thickness and position of the implant, and guide the laboratory technician with fabricating the right custom abutment and restoration. This can be communicated with study models, photos, specific instructions on contour requirements, and dimensions of the restoration.
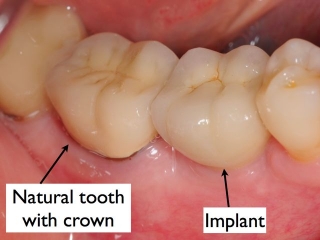
The result is a restoration that is aligned with adjacent teeth, well-supported soft tissue, better aesthetic outcome, and teeth that can be easily be cleaned by the patient.
Abutments by restorative dentists; Not surgeons!
Some surgeons have increasingly chosen to place the final abutments for their restorative dentists. This is largely a marketing strategy to make the implant process easier and cheaper for their restorative dentists, hence get more patient referrals in return. But many agree that this is highly inappropriate and not in the best interest of the patient and the final outcomes. The fact is the restorative dentists should be fully responsible for the abutment design, restorative design, and the overall restorative treatment.vThe surgeon should only be responsible for the proper foundation which includes creating proper bone and soft tissue dimensions and precise placement of the dental implants. The surgeon also should provide the restorative dentists critical information about implant stability and tissue quality to help the restorative dentists in their decision making process. Here are the reasons why restorative dentists, NOT the surgeons, should take full responsibility for the abutments and the restorations:
- Create proper abutment design- The restorative dentist should have full knowledge of patient’s occlusion, aesthetic requirements, anatomy of the supporting tissues, and condition of the adjacent teeth. Accordingly, the abutment must be designed to set the foundation for a restoration that has optimal functional and aesthetic features. This requires close collaboration between the restorative dentist and laboratory with specific instructions on abutment selection and design. The surgeon is not in the position to make such critical decisions.
- Optimize tissue support- A well designed abutment and crown supports the overlying soft tissue meeting the aesthetic and functional requirements. This translates into a more natural looking crown as well as one that can be easily cleaned by the patient. The restorative dentist knows what these requirements are and is better positioned to deliver them than the surgeon who has a more limited role.
- Create proper margins- The abutment margin must be carefully positioned (either at gingiva or slightly subgingival depending on the area) to keep tissues healthy and aesthetic. The restorative dentist is the right person to design the abutment in collaboration with his lab to accurately place the margins and achieve the desired results.
- Final crown anatomy- Implant dentistry is prosthetic based dentistry. The restorative dentist must know in advance the properties of the final restoration and be able to fabricate an abutment that meets those needs. A surgeon does not provide such treatments and while he can assist with the process, he or she is in no position to make the critical decisions on crown form and aesthetics.
- Whose fault in event of restorative complications? Restorative complications, while rare, do occur: crown loosening, abutment loosening, screw loosening, screw fractures, etc. Who is responsible to manage them? Will they have to be addressed by the surgeon who placed the original abutment or the restorative dentist who placed the crown? Is the surgeon knowledgeable enough to address such issues? The fact is when restorative dentists take control of the restorative needs including the abutment design and placement, there will be less complications. And should it happen, it will be clear who is in best position to address it.
While prefabricated abutments may be cheaper and quicker to do, they rarely provide the type of results that patients expect. Custom abutments are the best treatment option for all dental implant restorations. Further, it is best for restorative dentists to take full control of the restorative treatments including final abutment design and placement.
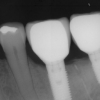
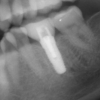
Lets look at the following examples: