Dental implants offer over a 98% success rate and are now the standard-of-care for replacement of missing teeth. To achieve life-time success, six critical and fundamental principles must be followed:
Have a Team of Dentists
The long-term success of dental implants requires collaborative efforts of at least two types of dentists, an oral surgeon and a restorative dentist. Placement of dental implants and its restorations (i.e. crown, bridge, denture) are two entirely different disciplines and it is virtually impossible for any one dentist to master both. A surgeon’s speciality and expertise allow him to properly develop the implant site and surgically place the implant in the right position while the restorative dentist will focus on making the implant supported crowns, bridges, or overdentures. Other types of dentists may be called upon for their expertise as needed. These include orthodontists, endodontists, and periodontists.
‘Fail to Plan; Plan to Fail’
During the Initial diagnosis and planning, both the surgeon and the restorative dentist must collaborate closely and evaluate the following: bone and gum tissue level and thickness; periodontal health; smile line; and the position of other teeth. This requires X-rays or other imaging techniques, a detailed examination, and study models which are all vital to a proper diagnosis. Study models can further be used for simulation of the final crowns, fabrication of a temporary prosthesis for the patient and making a special guide aiding the surgeon during implant placement. The surgeon and the restorative dentist, each with expertise in their field, should then review the gathered information and design a collaborative detailed plan to achieve a patient’s realistic goals. This plan, along with impending challenges, possible solutions, and associated risk factors should be thoroughly discussed with the patient. Team communication is vital to executing the plan and ultimate success.
Develop Proper Implant Bone Foundation
Extraction of a tooth consistently results in loss of bone and the overlying gum tissue. This can easily be prevented by making sure that the surgeon grafts the site at the time of the extraction. Preserving the bone also maintains the overlying gum tissue, therefore creating a healthy foundation for the implant and its crown. The graft materials most often used for this type of procedure are calcified granules supplied in individual containers, and it is rarely necessary to obtain it from the patient in the form of actual bone. These materials promote bone healing in an extraction socket and minimize its shrinkage. Another way to preserve the foundation is placement of the implant at the time of the extraction. This is known as an ‘immediate implant’ and can be done predictably in appropriate sites. Finally, the temporary prosthesis, whether removable like a flipper or fixed like a bonded temporary crown, needs to be carefully shaped to guide the gum tissue during its healing.
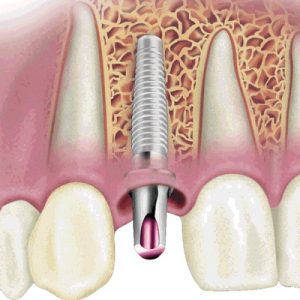
Precision Implant Placement
With a healthy foundation, the surgeon can now place the dental implant. But it is most crucial that the implant be positioned properly in all dimensions including height, width, and depth, and angulation. A poorly positioned implant is grounds for disaster and results in poor aesthetics and function. A simple rule is “To Never Place an Implant in the Wrong Position”. This is accomplished by using a surgical guide made on study models or by using CAT scan-generated computer plan. While the actual placement of a dental implant is simple, safe positioning and handling of the supporting tissue can be complex and should be performed by an experienced and skilled clinician.
Shaping the Gum Tissue
The gum tissue over the implant is next shaped by the placement of healing abutments (temporary extensions). For implants in the smile zone, the gum tissue must be shaped by the placement of a temporary crown on the implant. This is one of the most crucial steps and is often overlooked or rushed. It is the only way to create the desired gum tissue level and shape as well as provide a patient a ‘glance’ of what the final crown will look like. In some situations and if appropriate, an immediate temporary crown may be placed on the same day as the implant. Otherwise it may be placed several weeks later. Either way, the temporary crown should be left in place for 3-4 months to ‘design’ the proper gum tissue architecture as well as give the patient the opportunity to provide feedback on its appearance and comfort.
Final Prosthesis (crown, bridge, or denture)
The temporary crown provides a lot information that can be used to make the final crown look more natural, comfortable, and pleasing to the patient. Depending on the smile line, gum tissue thickness, and its shape, the restorative dentist may decide to use metal or ceramic extensions to support the final crown. Known as abutments, these extensions must have the proper contour to create a natural and healthy gum line and crown. It is crucial to use customized abutments that are fabricated in a laboratory, and not use ‘off-the-shelf’ abutments which are reshaped chair-side by the restorative dentist. It is the use of customized abutments that allow optimal gum tissue architecture, aesthetics, and crown fit. The final crown itself may be made of either porcelain with underlying metal or completely out of ceramic material. This decision must be made by the restorative dentist based on the aesthetic requirements of that specific patient. Finally it is important to use a quality laboratory and technicians who understand the demands of implants in the aesthetic zone and can work closely with the restorative dentist to make high quality crowns.
Your treatment may be staged in several phases or provided all at once. Your oral surgeon and restorative dentist will recommend the appropriate approach for you.