The Story:
Patient with pain, gingival swelling, and gum bleeding around an existing dental implant. Diagnostics included probing which revealed deep pocket and bleeding as well as both PA X-ray and CBCT that showed significant bone loss around the implant. A diagnosis of peri-implantitis was made but the cause could not be established.

Treatment
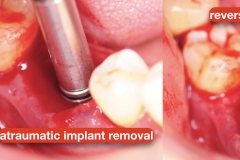
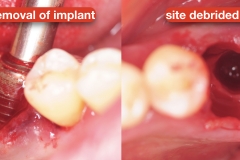
First the restoration was removed. Due to significant loss of attachment as well as poor placement, the implant was removed using atruamtic reverse torque explantation technique. With this approach, the implant is removed in a non-invasive technique without cutting the bone. The site was debrided and irrigated with saline. No grafting was done per patient’s preference.
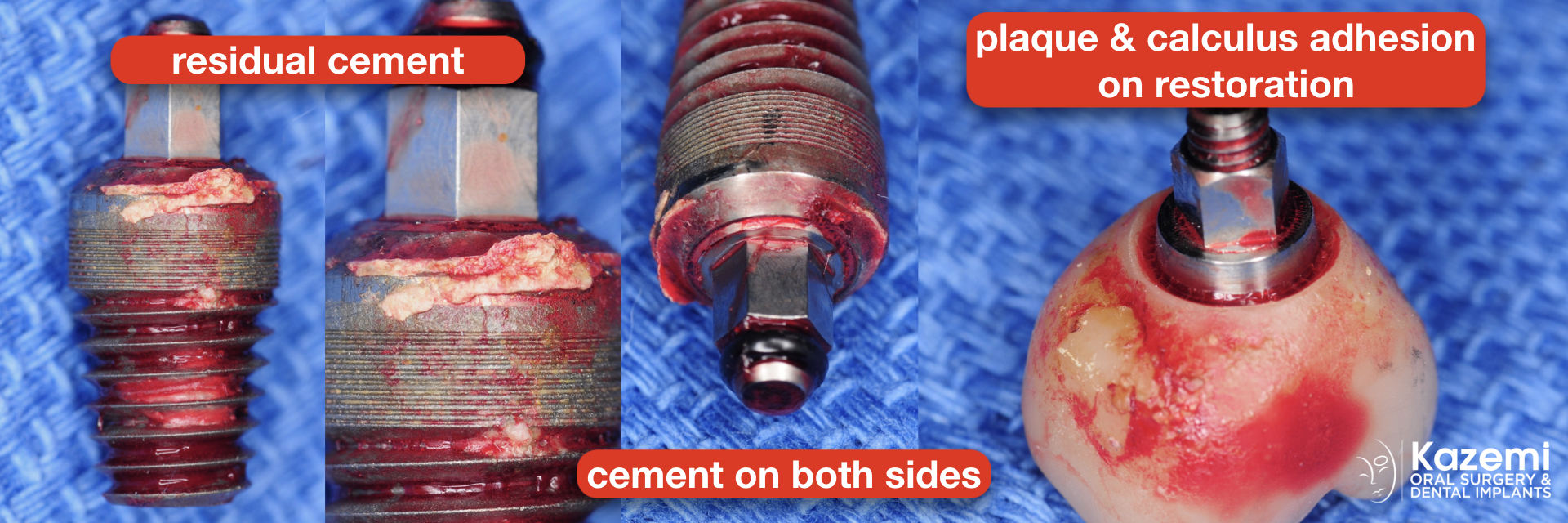
Cause of Peri-Implantitis
Close inspection of the implant showed residual cement as well as plaque and biofilm on the tissue surface of the restoration. Both are common causes of peri-implantitis.