The Story:
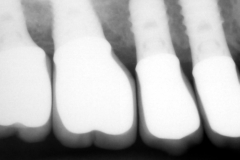
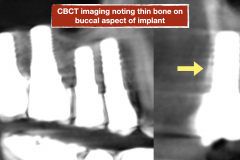
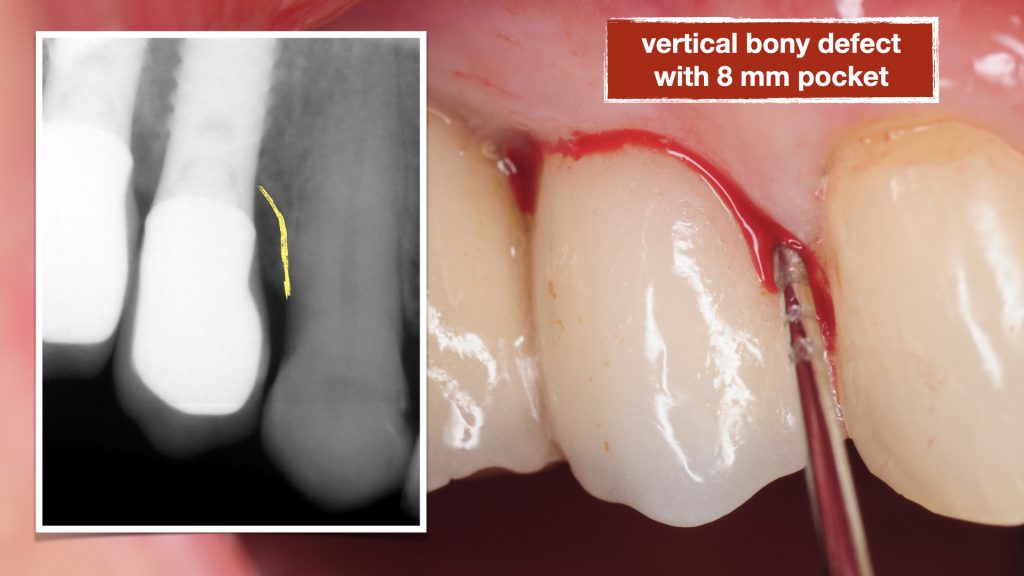
This patient presented to us with chronic pain around her dental implants that had been placed about 15 years prior. She had seen multiple dentists but could not achieve an explanation of her pain and was told the implants are healthy. On her initial visit, clinical examination was performed with probing and both conventional and 3-D X-rays (CBCT) were obtained for evaluation. Patient had 4 adjacent dental implants supporting single crowns. Evaluation showed a deep pocket between the most anterior implant adjacent to her natural tooth with pain and bleeding. This site with localized vertical bone defect showed significant inflammation and concluded to be the primary cause of her chronic pain.

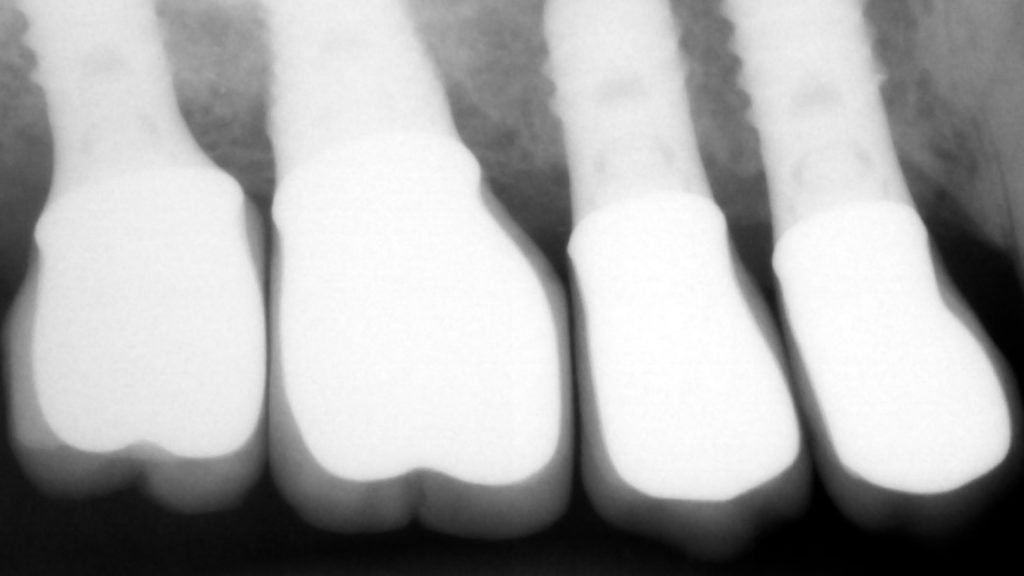
The implants were noted to be positioned deeper than her natural teeth, presumably because that’s where the bone was. The vertical discrepancy between the implant platform and the bone level around the natural tooth created a defect with deep pocket which made it very difficult to keep clean.
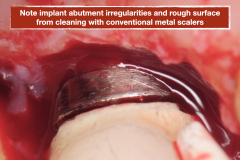
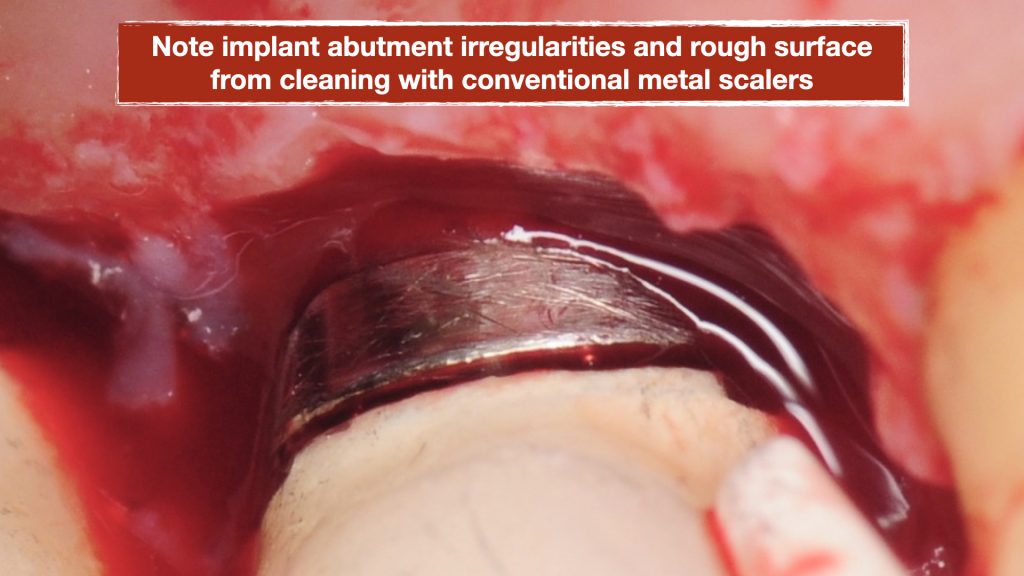
Additionally, the implant abutments were noted to have many gauges and rough surface from scalers and instruments that were inappropriately used during her cleanings. The rough surface increased plaque and biofilm retention which is impossible to remove and hence further contributing to the peri-implant mucositis (inflammation around implant). Also the margin of the crowns were noted to be open around the implant abutments creating additional areas of plaque trap.
Treatment
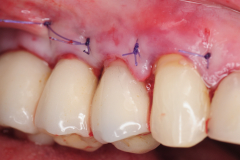
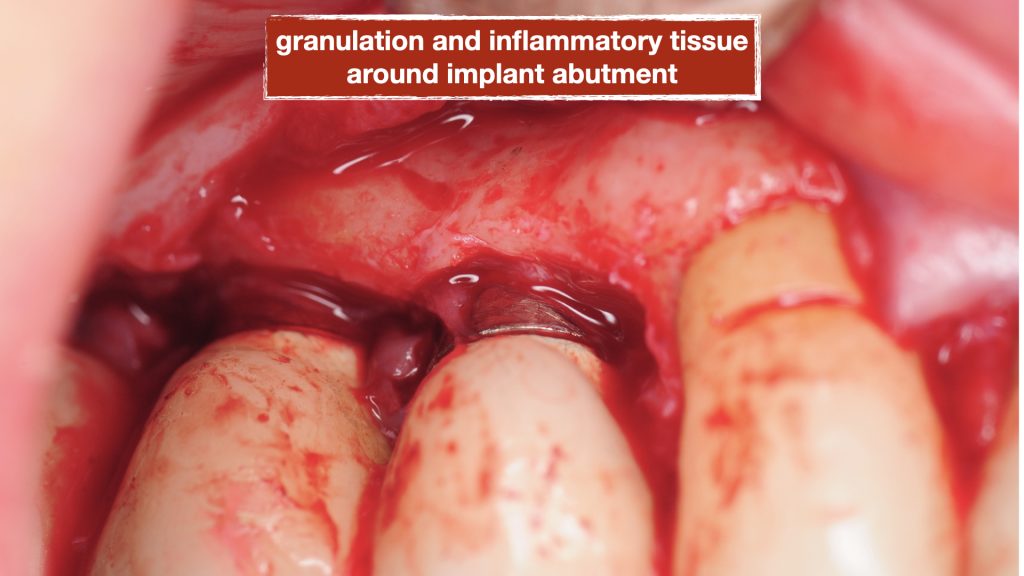
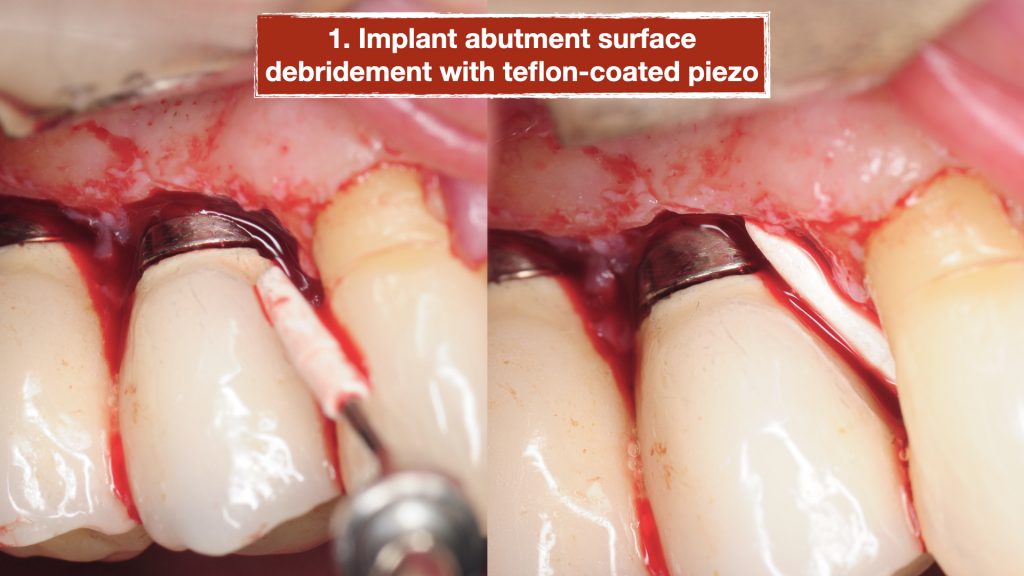
A surgical procedure was performed to explore the area and assess the condition of the implants more thoroughly. Following a gingival flap, inflammatory tissues were noted around the implant with the deep pockets. The implant surface was first cleaned using teflon-coated Piezo specifically designed for dental implants. Then the biofilm was removed using air/powder approach utilizing an Airflow Prophylaxis Master. Platelet rich fibrin membranes obtained from patient’s own blood was placed to provide autogenous growth factors for soft tissue healing and maturation. The gingival flap was then closed with resorbable sutures.

Outcome
Patient was closely monitored for 6 weeks. She reported significant decrease in her pain and symptoms. Her pain completely resolved after 3 months. While her symptoms had resolved patient was advised that the peri-implant mucositis could easily recur due to anatomic relationship of the implant to adjacent tooth as well as the rough surfaces of abutments and restorations. She was referred to a prosthodontist for evaluation of her abutments and crowns and consider replacement with new restorations. Additionally, patient was advised to seek professional cleaning using similar techniques as described above every 3 months and was given special instructions for home care.